GLP-1 Weight Loss: How to Protect Muscle, Strength & Long-Term Health
Why This Conversation Matters
Over the past year, medications like Ozempic (semaglutide) and other GLP-1 receptor agonists have moved from specialty clinics into everyday conversation. For many people, these medications have been genuinely life-changing. They quiet constant food noise, reduce appetite, improve blood sugar control, and help people finally gain traction in their health journey.
At the same time, across clinics, gyms, and the broader medical system, a growing pattern is emerging: people are losing weight quickly on these medications while also losing muscle, strength, and physical capacity at a rate that often goes unnoticed until problems appear.
This is not a fringe issue. It is a predictable physiological consequence of rapid weight loss. Ignoring it places long-term health at risk.
What These Medications Do — And the Trade-Offs
GLP-1 medications suppress appetite, slow digestion, and improve insulin signaling. They were originally developed for type 2 diabetes and are now widely used for weight management.
Their benefit is clear, they make it easier to eat less. The trade-off is equally clear, when calorie intake drops sharply, the body pulls energy from both fat and muscle tissue unless muscle is actively protected.
This is where many people get into trouble.
What Happens to Muscle During Rapid Weight Loss
A 2024 systematic review examining semaglutide’s effect on lean mass found that although fat loss is substantial, loss of lean tissue — including skeletal muscle — occurs consistently across clinical trials, in some cases making up a significant portion of total weight lost (Bikou et al., 2024).
Additional research suggests that 20–40% of total weight loss on GLP-1 medications may come from lean mass, a range similar to that seen after bariatric surgery and during aging-related muscle decline.
That level of muscle loss is not harmless.
Why Muscle Loss Is a Serious Health Issue
Muscle is one of the body’s most important protective tissues. It stabilizes joints, supports the spine, regulates blood sugar, maintains metabolic rate, protects against falls, and preserves independence.
When muscle declines, the body becomes:
weaker
slower
less stable
more injury-prone
metabolically compromised
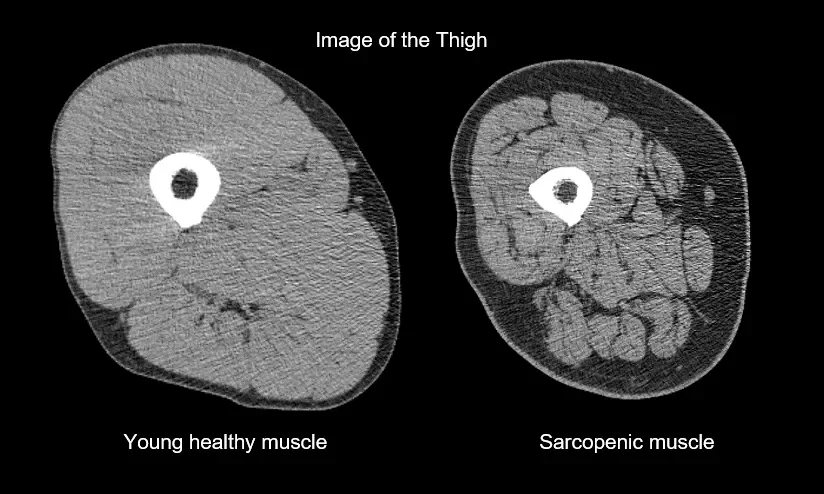
This process is known as sarcopenia — the progressive loss of muscle mass and strength. While commonly associated with aging, sarcopenia can be accelerated at any age by rapid weight loss when muscle is not intentionally protected.
Unchecked sarcopenia increases fall risk, worsens metabolic disease, reduces quality of life, and shortens healthspan.
Early Signs You May Be Losing Muscle on GLP-1 Medications
Many people assume muscle loss only shows up as “looking smaller,” but the earliest signs are usually functional:
feeling weaker in movements that used to feel easy
faster fatigue during normal activities
joint discomfort that wasn’t there before
difficulty with stairs, getting up from the floor, or carrying groceries
declining balance or coordination
These changes often appear before major visual changes occur and should be addressed early.
Who Is Most Vulnerable to Muscle Loss on GLP-1s
Some groups are at higher risk:
adults over 40
women (especially peri- and post-menopausal)
people with long periods of dieting history
individuals with joint pain or limited movement
those doing little or no resistance training
These individuals should treat muscle preservation as a medical priority, not a fitness preference.
Why Cardio Alone Is Not Enough
Cardio improves heart health and burns calories, but it does not provide the mechanical stimulus necessary to preserve muscle during calorie restriction. When weight loss is driven by appetite suppression and paired only with cardio, the body has no reason to keep muscle tissue. Resistance training is the signal that muscle is still required.
The Rebound Problem No One Likes to Talk About
Another major concern appears when people stop GLP-1 medications. Weight regain is common, but the regained weight is disproportionately fat, not muscle. The result is a body with higher fat mass and lower muscle mass than before treatment — a much more dangerous metabolic profile than the one that existed originally.
This pattern helps explain why many individuals feel weaker, stiffer, and less capable after stopping the medication, even if their weight is similar to where it started.
How to Use These Medications Without Sacrificing Your Body
Appetite suppression often leads to severe under-eating, especially of protein. Without adequate fuel, the body cannot maintain muscle regardless of how “good” the medication works.
Most individuals require approximately 1.2–2.0 g of protein per kilogram of body weight per day during weight loss to protect lean mass, along with sufficient total calories and micronutrients to support recovery and hormonal function.
If You Are Using a GLP-1 Medication, These Are Non-Negotiables
lift weights at least 2–3x per week
prioritize protein at every meal
do not allow prolonged periods of under-eating
monitor strength and function, not just scale weight
involve a professional who understands movement and load management
The Bottom Line
GLP-1 medications can assist with weight loss. They cannot protect your strength, your joints, your metabolism, or your future mobility.
That responsibility belongs to training, movement, and nutrition. Weight loss that sacrifices muscle is not progress — it is debt that the body will eventually collect.
At Six20 Strength, our role is to make sure that does not happen.
Sources:
Bikou A, Dermiki-Gkana F, Penteris M, Constantinides TK, Kontogiorgis C. A systematic review of the effect of semaglutide on lean mass: insights from clinical trials. Expert Opin Pharmacother. 2024 Apr;25(5):611-619. doi: 10.1080/14656566.2024.2343092. Epub 2024 Apr 18. PMID: 38629387.
Karasawa, T., et al. (2023). Unexpected effects of semaglutide on skeletal muscle mass and force-generating capacity in mice. Cell Metabolism, 37(8), 1619–1620.
Neeland IJ, Linge J, Birkenfeld AL. Changes in lean body mass with glucagon-like peptide-1-based therapies and mitigation strategies. Diabetes Obes Metab. 2024 Sep;26 Suppl 4:16-27. doi: 10.1111/dom.15728. Epub 2024 Jun 27. PMID: 38937282.
Muscle matters: the effects of medically induced weight loss on skeletal muscle. Prado, Carla M et al., The Lancet Diabetes & Endocrinology, Volume 12, Issue 11, 785 - 787